Abstract
- Issue: Federal financing for contraceptives is shown to enhance people’s access to these critical family-planning tools and improve their health and economic outcomes. Recent cuts to core federal programs, however, pose significant threats to both.
- Goals: Analyze the landscape of public funding for contraceptives and identify policies that undermine or expand equity, access, and choice.
- Methods: Expert interviews, literature review, and analyses of Medicaid state plan amendments (SPAs), Section 1115 waivers, managed care organization (MCO) contracts, state action plans, and Family Planning Annual Reports from the U.S. Department of Health and Human Services Office of Population Affairs.
- Key Findings and Conclusions: Federal programs, which are vital access points for contraceptives, face significant challenges related to the politicization of safety-net programs and contraceptives. However, with sufficient funding and creativity, states can utilize Medicaid SPAs and Section 1115 waivers, MCO contracts, and Title X and Title V grants to expand access. Despite the challenges they face, each program serves a unique purpose by utilizing different operational mechanisms. Still, gaps in access to contraceptives persist, and efforts to cut, restrict, or consolidate programs will result in poorer access.
Introduction
Contraceptives, including condoms, the birth control pill, and long-acting reversible contraceptives (LARCs), are a vital part of reproductive health and family planning. Since the first oral contraceptive was approved by the Food and Drug Administration (FDA) in 1960, millions of people have benefitted from greater control and autonomy over their reproductive decisions. In addition to being a core component of pregnancy prevention and planning, contraception can be used as part of treatment plans for conditions such as polycystic ovary syndrome and endometriosis.1
Access to contraception is positively tied to other health outcomes, including lower maternal and infant mortality rates, reduced preterm births, and lower rates of reproductive cancers.2 Research suggests that contraceptive access improves economic and educational outcomes for women — including 20 percent higher college enrollment, higher wages, and lower rates of poverty.3 In 2024, eight in 10 women of reproductive age, or ages 18 to 49, reported using some form of contraception in the previous 12 months, and four in five Americans supported legislation to protect access.4 As well as being politically popular, contraceptives are cost effective: every dollar spent on contraceptive services saves nearly six dollars in public spending.5
Despite broad support, Americans experience significant disparities in contraceptive access and choice, leading to deep health inequities. Public programs such as Medicaid, the Title X Family Planning Program (Title X), and the Title V Maternal and Child Health Services Block Grant Program (Title V) — which support clinics, services, and programs that deliver care to patients — are critical to the contraceptive access infrastructure in the United States. In 2020, 7.2 million women received publicly supported contraceptive services.6 However, federal investment in contraceptives is still insufficient — more than 19 million women across every U.S. state live in a contraceptive desert, meaning they lack reasonable access to a health center offering the full range of contraceptive methods.7 Legislative and judicial efforts that threaten access to abortion also pose serious threats to contraceptive access. A growing body of evidence suggests such abortion restrictions result in provider closures, reduced care quality, and increased delays to accessing care at all.8
Closing gaps in contraceptive access requires robust investment in public programs that are adequately funded, with flexibility for states to offer the services their constituencies need and protections to ensure high-quality and evidence-based care. Federal programs have long played a key role in working toward contraceptive equity, where people of any background or identity have reliable and uncoerced access to, and choice of, the full range of methods. However, threats to these programs are likely to further entrench systemic injustices.
This brief offers a roadmap for policymakers and advocates by analyzing the landscape of federal public financing for contraceptives, identifying opportunities for states to leverage federal systems for additional resources, and identifying challenges to maintaining and expanding contraceptive access through federal funding.
Landscape of Federal Financing for Contraceptive Access
Medicaid, Title X, and Title V are the most prominent federal programs supporting contraceptive access and equity.
Medicaid. Medicaid is the largest source of public funding for family planning services, a mandatory benefit in the program. The services that states must offer under “family planning,” however, remain ambiguous, which contributes to variability in contraceptive care across states.9 In 2023, the program covered over 83 million people in the United States, including 13.5 million (20 percent) women of reproductive age (18–49), of whom nearly 9 million (44 percent) have incomes below 200 percent of the federal poverty level.10
Some states have expanded access to contraceptives through state plan amendments (SPAs), which create permanent changes to state Medicaid programs, and Section 1115 waivers, which allow states to temporarily test demonstration projects. Some states also include language in Medicaid managed care contracts that impact contraceptive access, coverage, and choice.
Title X. Created in 1970, the Title X Family Planning Program is the only federal government grant program dedicated to family planning.11 Funding is determined annually by Congress and distributed by the U.S. Department of Health and Human Services (HHS) to states, local public health departments, and nonprofit health providers — each of which can divide funds between approved subgrantees.12 In 2023, Title X funded 3,853 health centers which served 2.8 million people in every state and territory.13
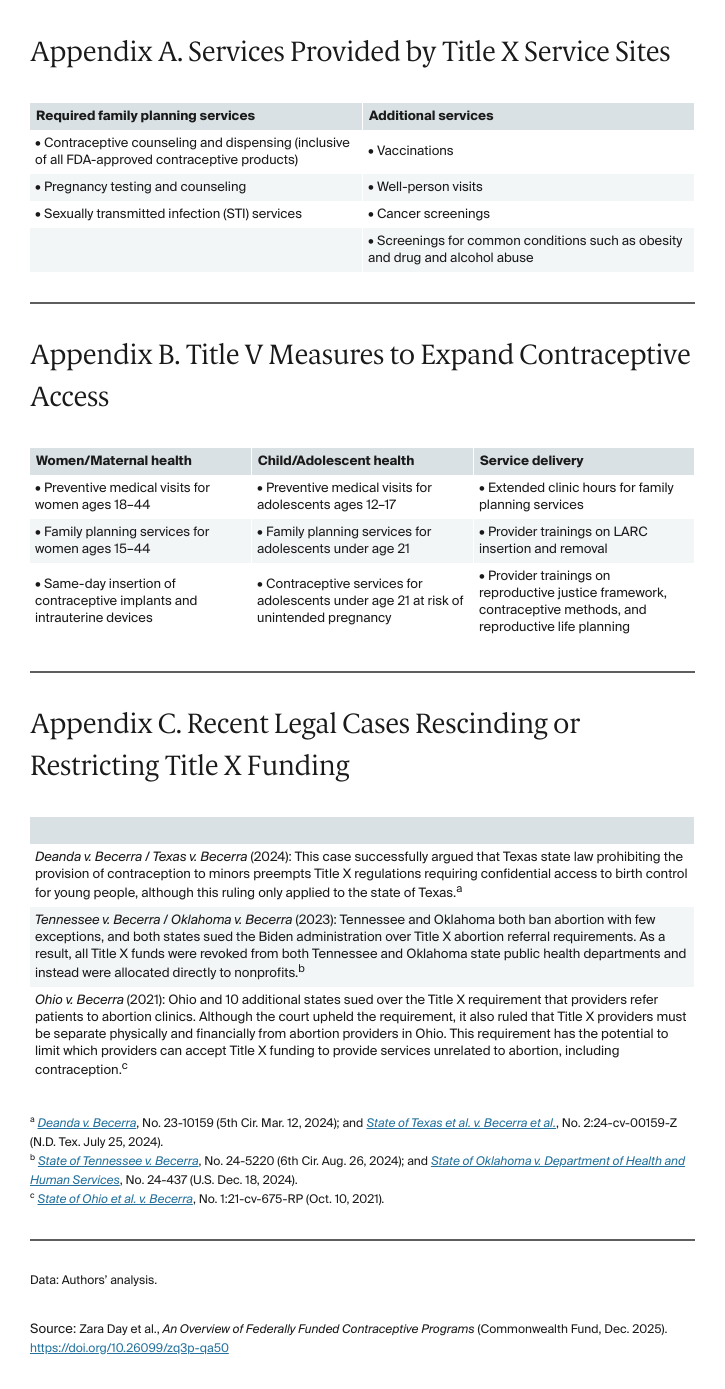
In addition to providing family planning services, Title X–funded health centers are critical sources of primary care (see Appendix A for services).14 Patients with incomes at or below the federal poverty level do not pay for their care, and those above pay on a sliding scale.15 One 2016 study found these centers to be the only source of health care for 60 percent of their patients.16
Title V. Title V of the Social Security Act is a federal program aimed at improving the health of mothers and children. The Maternal and Child Health (MCH) Services Block Grant is the bedrock of the Title V program and reached an estimated 59 million women and children in 2023.17 While the MCH Services Block Grant is permanently authorized to be funded up to $850 million per fiscal year under Title V of the Social Security Act, enacted funding is discretionary and determined through the congressional appropriations process each year.18 Once funding is appropriated, HHS allocates funding to state and territory applicants based on population size and need for MCH services.
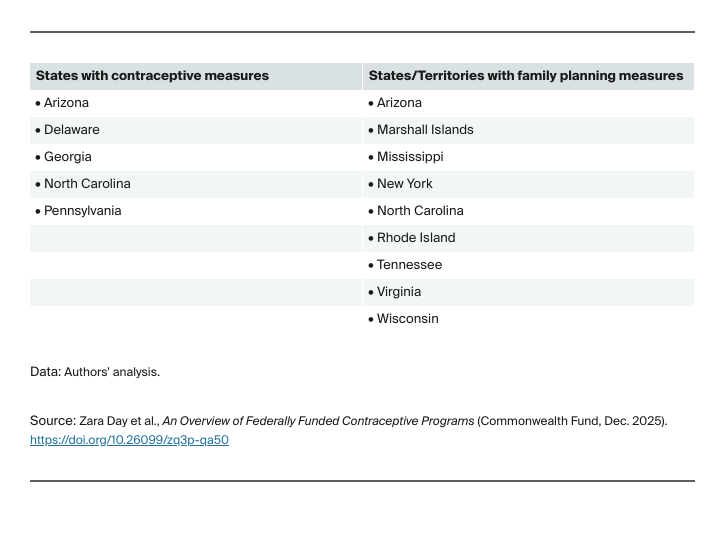
States and territories have flexibility to determine the best use of funding, including for direct and indirect health care services, workforce trainings, case management services, public health infrastructure and campaigns, and more.19 While there are no service requirements under the block grant, some states are integrating measures that focus on family planning and contraceptive access. Appendix B highlights some of the family planning and contraceptive services and practices that states prioritize to meet the needs of their communities.
Key Findings
Medicaid provides unique flexibility for states to expand contraceptive access.
Three existing Medicaid mechanisms can be leveraged to increase contraceptive access, equity, and choice:
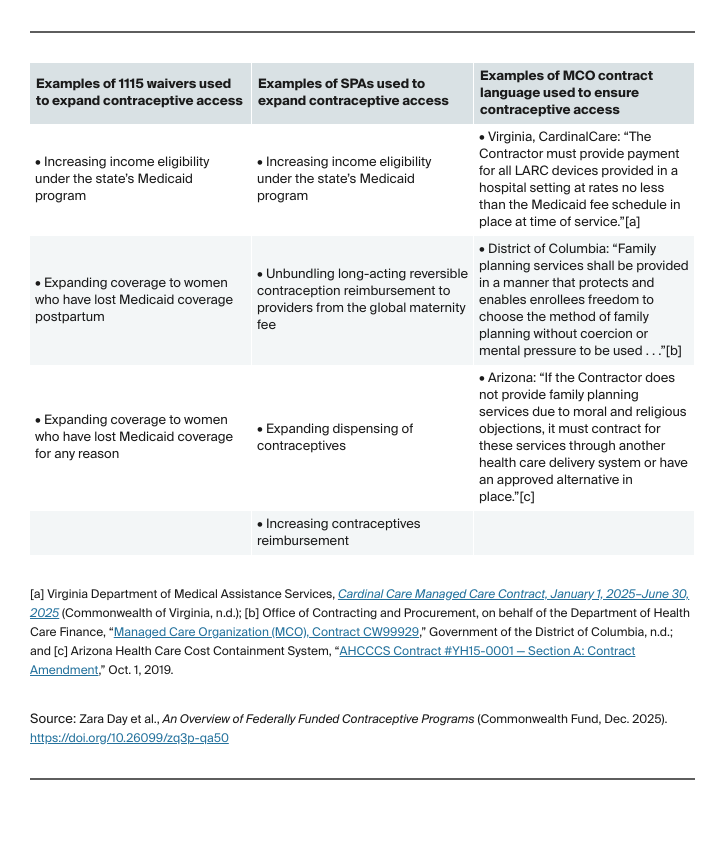
- Section 1115 waivers are primarily used to temporarily change or expand coverage for specific populations or select services.
- SPAs are often mutually exclusive from Section 1115 waivers but can be used to permanently achieve many of the same goals.
- Medicaid managed care contract language can be leveraged regardless of a state’s use of SPAs or waivers. Contract language can be used to shape the communication and delivery of care requirements, or to ensure that services meet evolving expectations or standards of care.
States can increase access to contraceptives by tailoring their Medicaid programs to best meet the needs of their constituents. Family planning expansions of all types can yield financial benefits for states and help reduce unplanned pregnancies.20
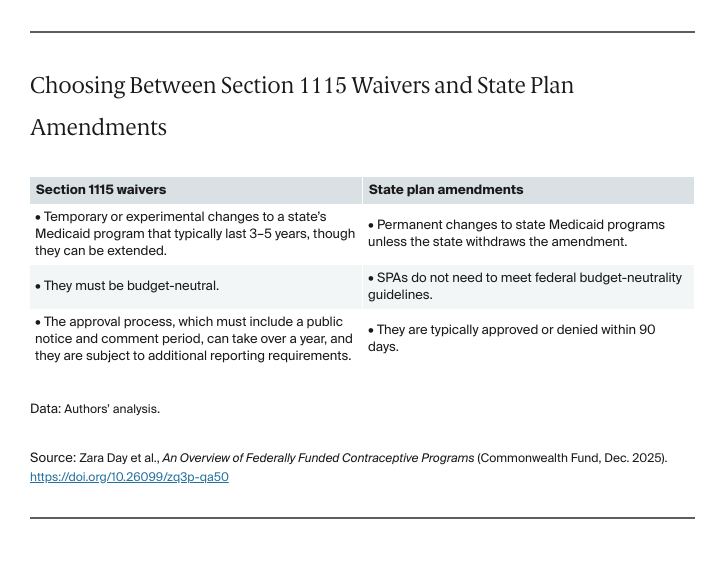
As of April 2025, 11 states have active family planning 1115 waivers that broaden eligibility by increasing income thresholds or expanding to women who have lost Medicaid coverage.21 While 1115 waivers have effectively increased access to contraceptives, they have limitations. Because waivers are not permanent — they require approval and renewal by the Centers for Medicare and Medicaid Services every three to five years — they are vulnerable from one administration to the next. Waivers also have long and onerous application and renewal processes with public comment periods.22
Some states have transitioned their 1115 waivers into SPAs, which create permanent changes to state Medicaid programs that are less vulnerable to volatility between administrations. A 2018 study found that women in states that transitioned from a 1115 waiver to an SPA were more likely to use postpartum contraception compared to those in states that did not transition.23 SPAs utilize a broader range of methods to expand contraceptive access than 1115 waivers. Many states have SPAs that expand access to family planning services by increasing the populations eligible for coverage, broadening provider payment and reimbursement structures, and optimizing how — and in what quantities — contraceptives are dispensed.
While 1115 waivers and SPAs can increase contraceptive access by, for example, expanding who is eligible for family planning services, states can also include certain requirements and contraceptive access language in their contracts with Medicaid managed care organizations (MCOs) in order to ensure that contraceptive access points meet evolving standards of care delivery. Seventy-five percent of people enrolled in Medicaid receive their care through MCOs.24 Some states currently use MCO contract language to increase access to contraceptives, including through incorporating requirements that members receive information and counseling for family planning methods, unbundling reimbursement for postpartum LARCs, or ensuring members can choose a contraceptive method without coercion.25
Outside of 1115 waivers, SPAs, and MCO contract language, states have also leveraged legislation and rulemaking to allow for Medicaid coverage of over-the-counter contraceptive methods, including condoms or Opill, the first FDA-approved over-the-counter birth control pill. However, awareness, uptake, coverage gaps, and reimbursement issues present challenges to some of these expansions.
Title X fills different gaps than Medicaid.
Title X funding is critical to expanding access to contraceptive care, including for people who have low incomes and are without health coverage. While Medicaid is a mandatory spending program, Title X funding is discretionary and must be adjudicated by Congress every year. Since 2015, however, annual funding has remained flat, at $286 million, despite demand for family planning services surpassing available funds year over year.26
Breaking with precedent, proposals for FY 2026 went as far as to eliminate the program: President Trump’s fiscal year 2026 budget funded Title X at zero dollars, and the House of Representatives mirrored this request in their funding proposal.27 The Senate’s funding proposal remained at $286 million.28 The difference between these two chambers’ proposals must be resolved in order for Congress to pass an FY 2026 health funding bill, which is still in progress as of publication.
Given the role of HHS in implementation, the administration holds significant power in program design and grantee operations. The increasingly partisan nature of family planning policy has led to dramatic fluctuations between administrations, which have significantly undermined the capacity of Title X health centers to provide quality family planning services.