Abstract
- Issue: Without national, validated standards for measuring disparities in health care, rating, ranking, and regulatory organizations have adopted different metrics and methodologies for evaluating progress. Inconsistent measurement tools can draw incomplete or even conflicting accounts of an organization’s progress toward health equity and risk curbing the advancement of efforts to achieve equity.
- Goal: To investigate the current state of health equity metrics across rating and regulatory entities and propose a set of guiding principles for evaluating institutional progress.
- Methods: Systematic evaluation of the methodologies of current and proposed health equity metrics across rating and regulatory organizations.
- Key Findings and Conclusions: The lack of standardization across rating and regulatory health equity metrics may undermine efforts to achieve equity. Metrics and methodologies must be aligned to accurately assess health equity progress and drive institutional change and improvements for patient populations.
Introduction
Structural racism, poverty, and inequities in housing, education, and employment have created significant gaps in health outcomes.1 Unequal rates of disease, treatment, and mortality disproportionately affect marginalized communities. During the COVID-19 pandemic, for instance, Black, Latina and Latino, and Native American communities suffered disproportionately high death rates, underscoring the longstanding effects of these systemic inequities.2 This reality catalyzed urgent calls to address systemic drivers of health disparities and to elevate equity as a cornerstone of health care.
The Robert Wood Johnson Foundation defines health equity as “everyone [having] a fair and just opportunity to be as healthy as possible. This requires removing obstacles to health such as poverty, discrimination, and their consequences, including powerlessness and lack of access to good jobs with fair pay, quality education and housing, safe environments, and health care.”3 Some health care organizations have started incorporating health equity into their strategies through community-based initiatives, local procurement and hiring, equity-focused research, and political advocacy. However, while various national organizations have proposed different approaches to measuring progress toward equity goals in the health care sector, there is not yet an agreed upon, nationally validated standard of measurement. Inconsistent methodologies and tools for evaluating progress can produce incomplete or even conflicting accounts of an organization’s progress toward health equity. Hastily applied metrics also could cause more harm or confusion than good by inaccurately measuring success.4 Aligning around health equity metrics is an urgent task in addressing longstanding racial, ethnic, and economic inequities in health care.
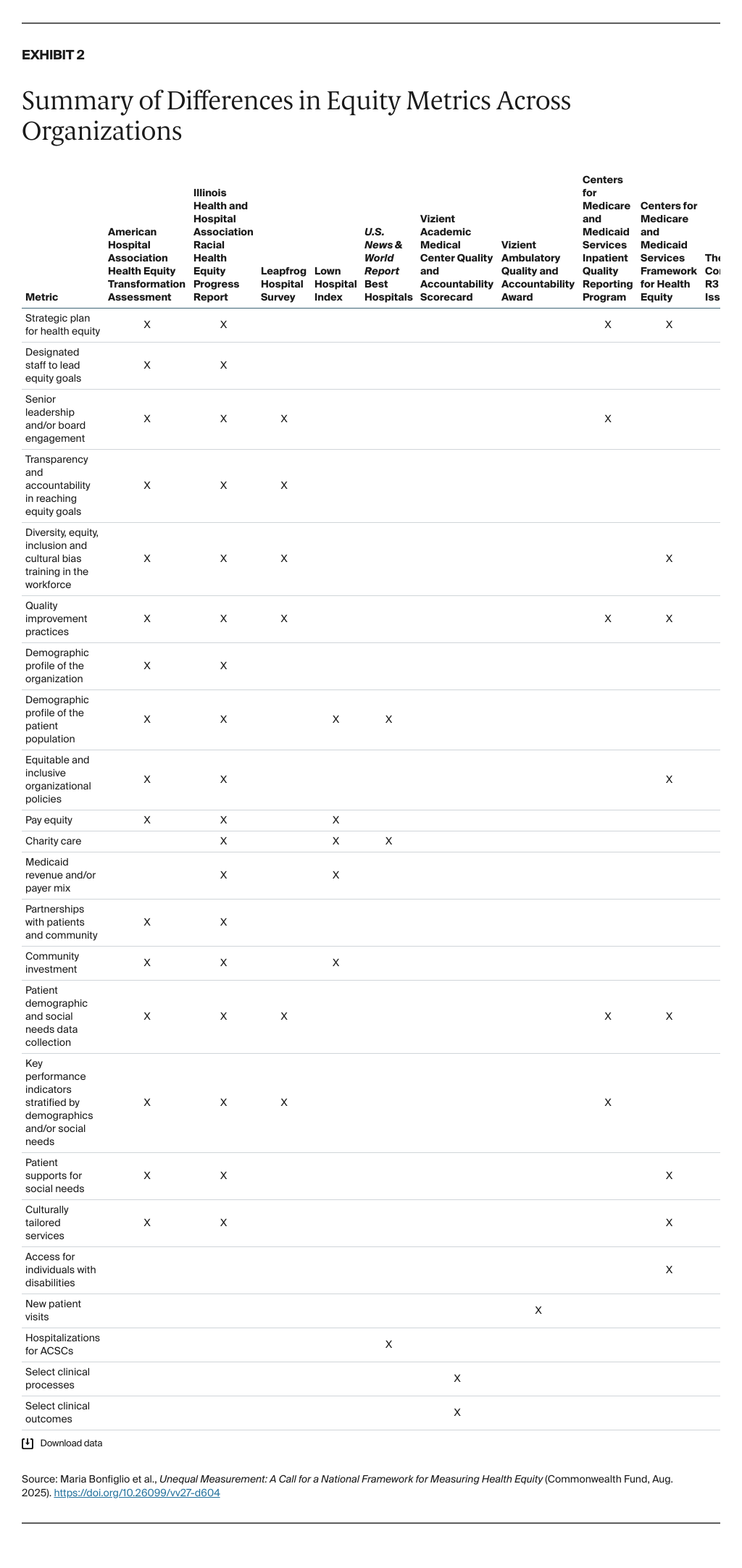
This brief assesses frameworks and metrics developed by eight of the biggest drivers of health care quality and equity, including Centers for Medicare and Medicaid Services, The Joint Commission, and prominent hospital rating and ranking organizations like U.S. News & World Report (USNWR). A side-by-side comparison of these organizations’ measures reveal a lack of consensus around health equity progress. Based on this analysis, we developed guiding principles for measuring and validating institutional progress toward addressing health disparities and achieving health equity.
Existing and Proposed Health Equity Metrics
Current health equity measures and frameworks do not lend themselves to simple categorization or comparison because of the wide variation between them. Frameworks can rely on qualitative or quantitative measurements, and they can focus on only health care delivery and quality or look at broader domains such as community, organizational leadership, patient care, and employees. Some frameworks utilize publicly available, population-level data, which is influenced by a variety of factors — such as pollution, housing conditions, transportation access, socioeconomic status, education, cultural beliefs, discrimination, and social support networks — that may not always be accounted for in the analysis. Others require detailed assessment of processes and performance at the organizational level.
Our sample of the most well-recognized, hospital-based health equity frameworks and assessments are divided into four distinct categories based on data type and scope: 1) those that use self-reported qualitative and quantitative data at the organizational level across multiple domains like community, strategy, and policy; 2) those that use regulatory frameworks across multiple domains; 3) those that use administrative data across multiple domains; and 4) those that use quantitative data over a single domain (see Exhibit 1 for an overview).

Organizations Using Self-Reported Qualitative and Quantitative Data Across Multiple Domains
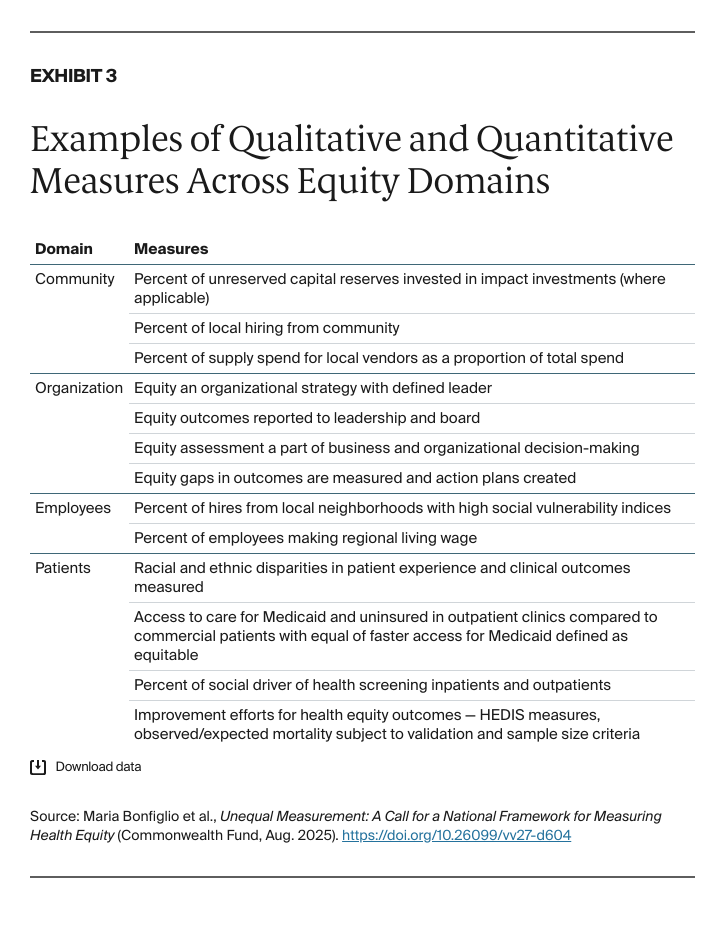
The 2023 Illinois Health and Hospital Association’s Racial Health Equity Progress Report (IHA Progress Report)5 comprises 10 composite metrics across four domains:
- community
- organization
- people (employees)
- patients.
Measures include comparison of organization board and leadership demographics, community and patient demographics, diversity and inclusion in the workforce, leadership engagement in health equity, patient assessments regarding experience and health outcomes, patient supports for drivers of health screening, access to free and discounted care, community investment, and community partnerships. The assessment includes 32 questions, 15 of which include open-ended follow-up questions. Open-ended questions are not scored; they are intended to prompt organizations to reflect on ways to improve their processes. Each health care organization receives a composite score. The assessment is widely available nationally6 for all health care organizations through a Commonwealth Fund–supported project.
The 2023 American Hospital Association Health Equity Transformational Assessment (HETA)7 includes six measure domains:
- equitable and inclusive organizational policies
- data collection and use
- diverse representation in leadership
- community collaboration
- accountability
- culturally appropriate care.
The assessment includes 102 questions, many with multiple answer options. Participating organizations receive access to a dashboard with hospital positions along each domain of health equity, but no scores or ranks are assigned.
Leapfrog’s 2023 Hospital Survey8 includes an unscored health equity section comprising 13 questions. These questions are qualitative and quantitative, falling under the following domains:
- patient demographic data collection, validation, and staff training
- quality measure stratification and improvement
- transparency in health care disparities and equity initiatives
- board engagement
- unconscious and implicit bias training for staff.
Organizations Using Regulatory Frameworks Across Multiple Domains
In 2023, the Centers for Medicare and Medicaid Services (CMS) included the Hospital Commitment to Health Equity performance measure in their Inpatient Quality Reporting (IQR) Program and structured a Health Equity Framework9 for hospitals to guide their equity initiatives. The IQR performance measures include five structural attestations and one social needs measure. Hospitals need to attest that:
- equity is a strategic priority
- data are being collected to measure health equity
- data analysis is being performed to measure gaps in equity
- equity outcomes are included in the quality improvement initiatives
- there is demonstrable leadership engagement in health equity.
The social needs measure includes screening for social drivers of health among adult patients over age 18 hospitalized within acute care hospitals in the United States. Hospitals report on the screening and positivity rates.10
The Joint Commission’s standards for health equity11 were included within the National Patient Safety Goals, effective July 1, 2023. These standards will be evaluated as part of leadership criteria during triennial accreditation surveys. These requirements aim to ensure that:
- health equity is a quality and safety priority
- patient medical records capture social needs data
- hospitals are accountable and transparent in addressing disparities in care
- hospitals can demonstrate progress toward achieving equity goals.
Organizations Using Administrative Data Across Multiple Domains
The 2024–2025 USNWR health equity metrics12 incorporate three domains related to health care access, including social representation in access to care, racial disparities and time spent at home, and charity care provision for uninsured patients.
USNWR examines social representation in access to care by evaluating how Medicaid patients from the surrounding community are represented in the hospital’s patient population after accounting for specific community and hospital-level factors, the percentage of patients served who live in vulnerable neighborhoods, and the representation of non-white populations from the surrounding community in the hospital’s elective procedure patient population. In determining racial disparities and time spent at home, USNWR uses claims-based data to evaluate the difference in number of days that a patient spent at home within 30 days of discharge, for Black patients compared to white patients for orthopedic and cardiac procedures. In evaluating charity care, USNWR looks at provisions for the uninsured compared to the hospital service area uninsured population by reviewing reporting on hospital 990 IRS submissions. Lastly, the ratios of Medicaid discharges and racial and ethnic patient percentages were compared to those proportions with Medicaid within the hospital service area.
The 2022 Lown Institute Hospitals Index13 evaluates health equity across five domains:
- pay ratio of executives to staff without advanced degrees
- time spent on charity care
- community benefit as a proportion of total expenses
- Medicaid revenue as a share of total revenue
- hospital inclusivity, including a comparison of hospital patient income, education, and racial distribution to the community area.
Organizations receive an equity grade derived from a composite score along with a state and national rank.
Organizations Using Clinical Quantitative Data in a Single Domain
Vizient’s 2022 Quality and Accountability Scorecard14 narrows in on clinical performance and includes inpatient clinical process and outcome metrics for health systems and timeliness for new patients to be seen for ambulatory settings. Inpatient metrics include sepsis and shock lactate timing and observed over expected mortality, non-ST-Elevation myocardial infarction (NSTEMI) troponin timing and observed over expected mortality, maternal hemoglobin change and transfusion rate, and heart failure brain natriuretic peptide improvement and observed over expected mortality.
The scoring methods examined equality between sex, race, and payer groups for each metric, with maternal measures stratified by only race and payer. The Vizient ambulatory metric is a 10-day access metric which evaluates the time to be seen for new Medicaid and commercial patients by specialty.