Medicare Advantage (MA) plans offer supplemental benefits that are not included in traditional Medicare. These commonly include dental, vision, and hearing coverage, but can also involve services like meal delivery or transportation. In 2025, the Centers for Medicare and Medicaid Services (CMS) paid plans $39 billion to provide these extra benefits. Plans extensively market their supplemental benefits; one of four MA enrollees report choosing their plans over traditional Medicare because of them.
But many enrollees don’t use the extra benefits. In 2024, three of 10 MA beneficiaries reported not using any supplemental benefits in the past year. Less than half used dental, vision, gym memberships, or over-the-counter drug allowance benefits, and less than 10 percent used benefits like hearing, grocery allowance, or meal delivery. If the benefits are not used, the insurers are permitted to keep any unspent funds. This has raised questions about whether enrollees are aware of their benefits, if benefits are aligned with enrollees’ needs, if the benefits are leading to better health outcomes, and whether payments to plans for funding these benefits are being used most efficiently.
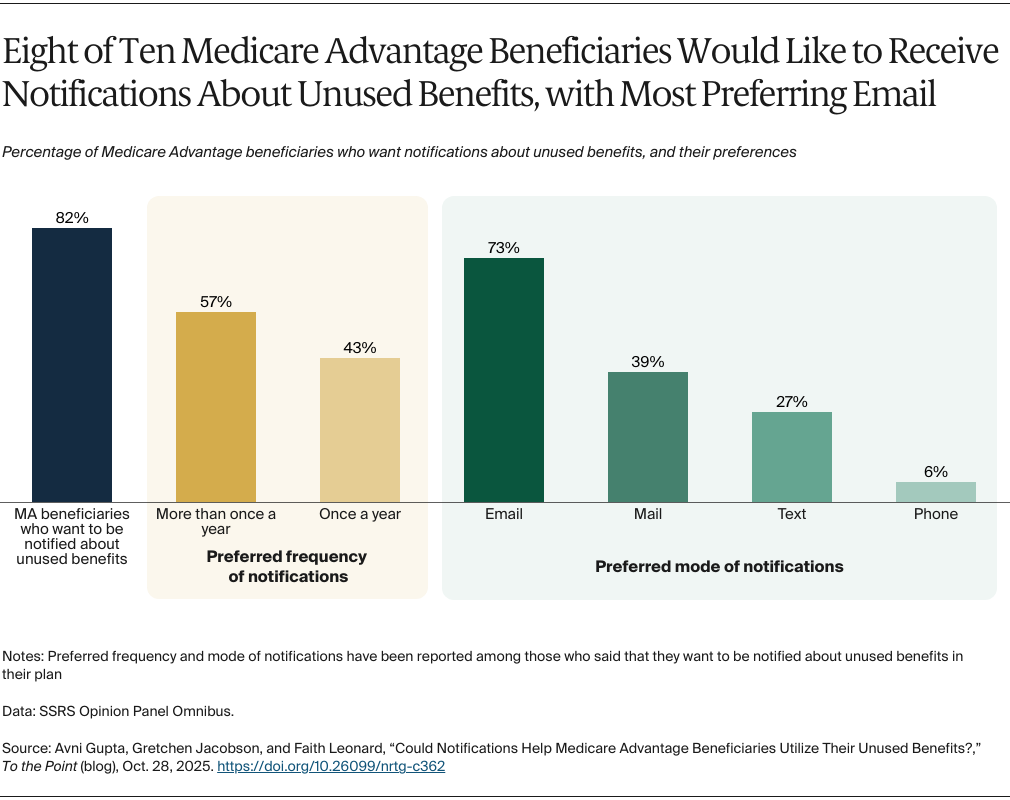
To learn more, the Commonwealth Fund and SSRS surveyed MA enrollees. The survey explored beneficiaries’ use of supplemental benefits, their reasons for not using them, and their views and preferences regarding notifications about unused benefits.
Two of Five MA Beneficiaries Don’t Plan to Use Some of Their Benefits
Two of five Medicare Advantage enrollees said they don’t plan to use some of their plan benefits. When asked why, 58 percent said it was because they don’t need them. More than one of five either said that they don’t know all the benefits (24%) or don’t know how to use them (21%). More enrollees with lower incomes (i.e., below $50,000), compared to those with higher incomes, said they don’t plan to use benefits because they don’t know how to use them (31% vs. 7%). Those with higher incomes were more likely to report not needing the benefits (70%) compared to enrollees with lower incomes (50%).