In July 2025, Congress passed H.R. 1, which cut more than $900 billion from Medicaid — the largest cuts in the program’s history — and is expected to cause more than 5 million individuals to become uninsured. For hospitals and providers, this will increase levels of uncompensated care while also decreasing overall revenue as reimbursement rates decline. The resulting budget shortages could cause hospitals and other health care facilities to close. The cuts will disproportionately affect rural areas, which have a higher proportion of Medicaid beneficiaries. Federal spending on Medicaid in rural areas is predicted to decrease by $137 billion over the next 10 years. The cuts will disproportionately impact states that expanded Medicaid as these states have larger Medicaid enrollment and thus will incur larger losses.
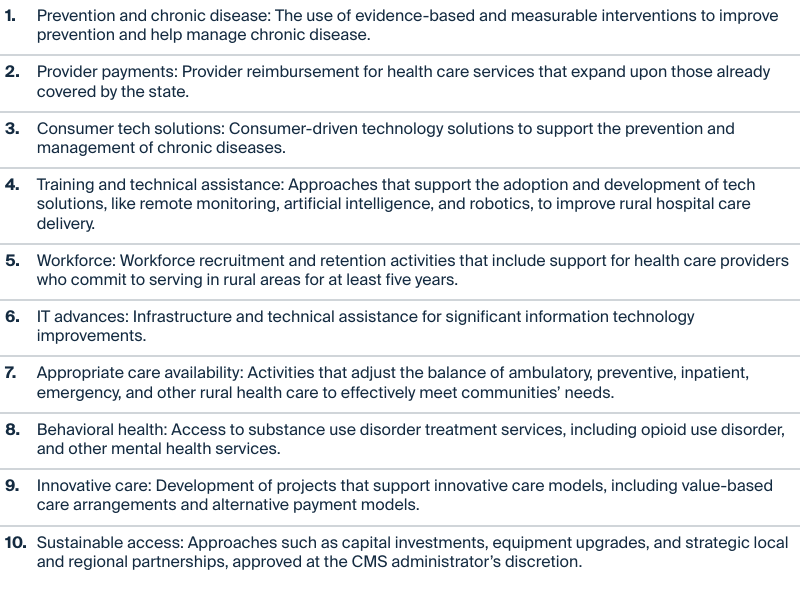
H.R. 1 also introduced the Rural Health Transformation Program, proposed by sponsors to help offset the impact on rural hospitals and providers. The resources available under the program favor the administration’s policy goals. This includes Make America Healthy Again priorities like instituting the President’s Physical Fitness Test, which uses competitions to encourage students’ physical condition and health; restricting the foods available under the Supplemental Nutrition Assistance Program (SNAP) by eliminating certain sugar-sweetened items; and encouraging patient engagement in health care through technology initiatives like allowing patients access to data and the use of technology wearables and health apps. The program gives the Centers for Medicare and Medicaid Services (CMS) administrator a high level of discretion in making funding decisions.
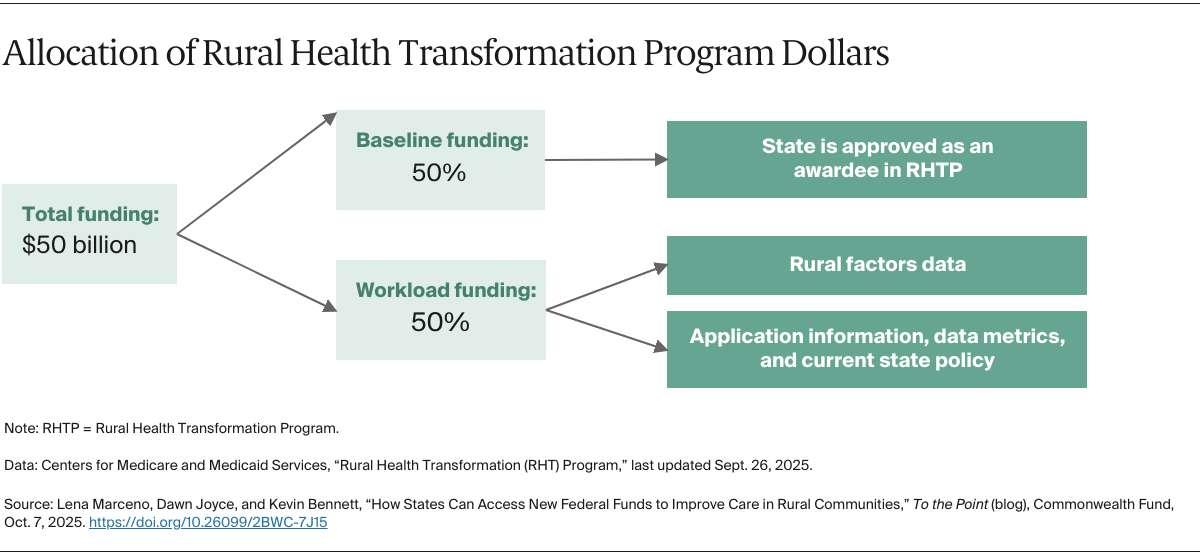
The program will invest $50 billion over five years, at a rate of $10 billion per year, starting in 2026. Half will be allocated equally to all states with approved applications; the other half will be determined by CMS based on factors outlined in H.R. 1 and further detailed in the Notice of Funding Opportunity (NOFO) released in September. To be considered for funding, states must submit their applications by November 5; CMS will announce awards by December 31. The program does not require states to contribute funds to the project.